A 69 year old female c/o of shortness of breathe and weakness since 2 days, fever(high grade) since 2 days hoarseness of voice since 10 days and cough since 1 week
Chief complaints -
69year old female resident of Nalgonda came to the OPD with chief Complaints of shortness of breath and weakness since 2 days,
fever(high grade) since 2 days
hoarseness of voice since 10 days and
cough since 1 week
History of Present Illness:
She was apparently asymptomatic 10 days ago, then started complaining of horseness of voice which began gradually
Cough since 1 week, dry in nature
Shortness of breath since 3 days (grade 1)
Fever high grade associated with chills since 1 day
History of Past illness:
H/o similar complaints in the last, 2 years ago, which relieved on medication.
No h/o TB
Known case of Hypertension since 5 years
Not a known case of DM, Asthma, Epilepsy,thyroid disorders.
No h/o inhaler usage in the past.
Personal History:
Daily routine- She used to wake up around 6am,have breakfast around 9am and then used to go to the shop. She used to have lunch at 1pm and would take rest for sometime and have dinner around 8pm.
Appetite: Normal
Diet: Vegetarian
Bowel movements: Regular
Micturition: Normal
Family History:
No significant family history
General Examination:
Patient is conscious, coherent cooperative and well oriented to time and place.
No signs of Pallor, Icterus, Cyanosis, Clubbing or
Generalised Lymphadenopathy.
Vitals:
Temp: 102 F
RR: 28/min
PR: 110/min
BP: 115/70mmHg
Sp O2 : 88%
GRBS: 160mg
Systemic Examination:
Respiratory system:
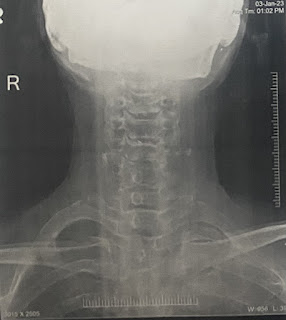
Position of trachea: central
Inspection:
Shape of chest- Barrel shape
Trachea central in position
Supraclavicular hallow- positive
Chest expansion- decreased movements
Spinoscapular distance equal on both sides.
No kyphosis/scoliosis
No sinuses, venous engorgements.
Palpation:
All inspectory findings are confirmed with palpation.
Apex beat - 2 cm medial to mid clavicular line
Tactile Vocal Fremitus is increased in left infraclavicular area
Antero-posterior diameter- 21cms
Transverse- 22cms
Percussion:
Tactile Vocal Fremitus is increased in left infraclavicular area
Right. Left
Supraclavicular Resonant. R
Infraclavicular. R. Dull
Mammary. R. R
Axillary. R R
Infra axillary. R R
Suprascapular. R R
Interscapular. R R
Infrascapular R R
Auscultation:
Right. Left
Supraclavicular. Normal vesicular NVBS
breathe sounds
Infraclavicular. NVBS. Tubular
Mammary. NVBS NVBS
Axillary. NVBS. NVBS
Infra axillary. NVBS. NVBS
Suprascapular. NVBS. NVBS
Interscapular. NVBS. NVBS
Infrascapular NVBS. NVBS
Cardiovascular Examination:
Thrills: no
Cardiac sounds: S1, S2 heard
Cardiac murmurs: No
Apex beat is found at 2cms medial to 5th intercoastal space.
CNS:-
Memory intact
Higher mental functions normal
Oral examination - dental caries on left lower molar is present
Provisional Diagnosis:
We might suspect Left upper lobe fibrosis or vocal cord palsy or maybe Malignancy of larynx.
Hypertension since 5years.
Treatment :
Inj.Augmentin 1.2mg IV
Tab.Azec 500mg OD
Inj.Neomol 10mg IV
Inj.Pantop 40mg IV
Tab.Paracetmol 650mg TID
Syrup.Grillinctus 2tbsp TID
Neb.Duolin 8 hourly


















Comments
Post a Comment